Scroll to:
Polymorphisms of CYP2C9 and VKORC1 genes and their association with calcification of heart valves in Chuvash patients with chronic rheumatic heart disease
https://doi.org/10.37489/2588-0527-2025-1-17-23
EDN: BXYGEA
Abstract
Relevance. Patients with chronic rheumatic heart disease (CRHD) often require warfarin, individual sensitivity to which is determined by polymorphisms of the CYP2C9 and VKORC1 genes. Warfarin use is associated with arterial calcification, which is explained by inhibition of the matrix protein MGP. This may be significant in CRHD, a characteristic feature of which is calcification of the heart valves.
Objective. To study the polymorphisms of CYP2C9 (C430T and A1075C), VKORC1 (−1639G>A), and their association with calcification of the heart valves in Chuvash patients with CRHD receiving warfarin.
Methods. The study included patients meeting the following criteria: 18–80 years old, confirmed CRHD, warfarin therapy, self-identification as an ethnic
Chuvash. Calcification of the valves was confirmed by echocardiography. Genotyping was performed by PCR.
Results. The frequency of the A allele of the VKORC1 gene (−1639G>A) was 48.60 %, the T allele (CYP2C9*2) — 10.15%, and the C allele (CYP2C9*3) — 4.05 %. Calcification of the heart valves was detected in 75.7 % of the examined patients: the aortic (50 %) and mitral (45.9 %) valves were most often affected, while the tricuspid valve was involved less often (4.1 %). Statistical analysis demonstrated a significant association between homozygous carriage of the VKORC1 (−1639G>A) allele A and the development of aortic valve calcification (p = 0.023), while the difference between the AA and GA groups also reached statistical significance (p = 0.021).
Conclusion. Identification of VKORC1 genetic variants, as well as the association of carriage of the A allele in homozygous form with valve calcification in patients with CRHD receiving warfarin therapy, can help in personalizing anticoagulant therapy, taking into account both the risks of hypocoagulation and the possible progression of heart valve calcification.
Keywords
For citations:
Georgieva K.S., Pavlova S.I. Polymorphisms of CYP2C9 and VKORC1 genes and their association with calcification of heart valves in Chuvash patients with chronic rheumatic heart disease. Pharmacogenetics and Pharmacogenomics. 2025;(1):17-23. (In Russ.) https://doi.org/10.37489/2588-0527-2025-1-17-23. EDN: BXYGEA
Introduction
Chronic rheumatic heart disease (CRHD) is a pathological process characterized by progressive structural changes in the heart valves that occur as a result of acute rheumatic fever. A feature of this disease is post-inflammatory marginal fibrous changes in the valve cusps with the development of deformation and loss of valve function. Morphological manifestations may include not only fibrosis, but also calcification of the tissues of the heart valves (especially mitral and aortic). As a result of such changes, characteristic valve deformations are formed: mitral stenosis and/or regurgitation, as well as aortic stenosis, which contributes to hemodynamic impairment and significantly worsens the quality of life of patients, often requiring surgical intervention. The high risk of thromboembolic complications due to the presence of possible pathological conditions such as atrial fibrillation, venous thrombosis and implantation of artificial heart valves necessitates the administration of anticoagulant therapy to patients with CRHD. Warfarin remains the most frequently prescribed anticoagulant for CRHD, and in the presence of mechanical valves it is the only alternative. Genetic variations, primarily polymorphisms of the CYP2C9 and VKORC1 genes, play a critical role in the efficacy and safety of warfarin therapy. The CYP2C9 gene encodes the cytochrome P450 enzyme, which is a key participant in warfarin metabolism. Carriage of allelic variants CYP2C9*2 and CYP2C9*3 is associated with a decrease in the catalytic activity of the enzyme, which leads to slow metabolism of warfarin. As a result, the likelihood of bleeding increases at standard doses [1, 2]. The VKORC1 gene encodes vitamin K epoxide reductase, a target of warfarin that plays a key role in vitamin K regeneration. In particular, VKORC1 catalyzes the reduction of the epoxide form of vitamin K, formed during γ-carboxylation of proteins, converting it into the active hydroquinone form. Due to this function, VKORC1 ensures the continuity of the vitamin K cycle, which is critical for post-translational modification of a number of proteins, including not only blood coagulation factors, but also matrix Gla proteins such as osteocalcin and MGP. Thus, genetic variations in VKORC1 can affect not only the coagulation hemostasis system, but also the calcification processes of various tissues [3].
The prevalence of VKORC1 alleles varies significantly in ethnic groups [4–22]. These differences are of great clinical importance, as they allow predicting the individual dose of anticoagulants, thereby minimizing the risk of bleeding. In addition, it has been demonstrated that the T allele of the VKORC1 polymorphism (1173C>T) is associated with a significantly higher risk of aortic wall calcification in representatives of the white race [23]. In this regard, we put forward a hypothesis about a possible relationship between the development of heart valve calcification and the carriage of VKORC1 gene polymorphisms (−1639G>A). According to the results of the All-Russian Population Census for 2020, the Chuvash population accounts for 0.82% and ranks fifth in size in Russia [24], however, information on the genetic status of the Chuvash is limited. In connection with the above, the aim of our study was to investigate the polymorphisms of the genes CYP2C9 (C430T and A1075C), VKORC1, and their association with calcification of the heart valves in Chuvash patients with CRHD. To achieve this goal, the following tasks were set: 1) to identify the frequency of polymorphic alleles among Chuvash patients with CRHD; 2) to study the prevalence of calcification of the valve apparatus among Chuvash patients with CRHD; 3) to study the association of carriage of polymorphisms of the studied genes with calcification of the heart valves in Chuvash patients with CRHD.
Materials and methods
A prospective study was conducted at the Republican Cardiology Dispensary of the Ministry of Health of the Chuvashia Republic (BRCD) from May 2023 to December 2024. The study included patients of the Chuvash population admitted to the hospital with the main diagnosis of CRHD. The study was approved by the local ethics committee of the Republican Clinical Oncology Dispensary of the Ministry of Health of the Chuvashia Republic (BRCD, extract from protocol No. 5 dated May 23, 2023). Informed consent was obtained from all patients in advance to participate in the study, as well as to the collection and storage of biomaterial. Ethnicity was determined by self-reference using an assessment of the genealogy of the study participant in two or more generations, and the absence of interethnic marriages. Criteria for inclusion and exclusion from the study were developed. The inclusion criteria for the study were:
- self-identification as an ethnic Chuvash;
- presence of an operated degenerative heart valve/valve defect or CRHD;
- warfarin therapy;
- inpatient treatment at the BUK "RKD" of the Ministry of Health of the Chechen Republic;
- patients aged 18-80 years.
The exclusion criteria were:
- self-identification as a patient not of the Chuvash ethnic group;
- chronic heart failure with an ejection fraction of less than 30%;
- chronic kidney disease stage 5;
- decompensated liver failure;
- malignant neoplasm of clinical groups 3-4 with the presence of distant metastases, lymphoproliferative diseases;
- septic condition of the patient / acute infectious process;
- acute cerebrovascular accidents;
- storage diseases (including amyloidosis);
- age over 80, under 18;
- grade 3 cerebrovascular insufficiency and/or mental illness;
- pregnancy.
To identify calcification of the heart valves in all patients included in the study, the results of echocardiography (EchoCG) and ultrasound examination (US) of the heart, conducted at the BUK "RKD", were analyzed. Genotyping was performed at the AU "RKOD". The material for determining polymorphisms was 4 ml of the patient's venous blood, collected from the cubital vein in test tubes with ethylenediaminetetraacetic acid. As part of the study, DNA was isolated and polymorphisms were determined by the polymerase chain reaction (PCR). For this, the Dtlite amplifier (OOO NPO DNA-Technology, Russia) and the PharmacoGenetics Warfarin reagent kit (registration number FSR 2010/08633 dated 01.07.24, OOO NPO DNA-Technology, Russia) were used. The kit included 48 tests, Taq-AT-polymerase, mineral oil, PCR buffer and tubes with the studied polymorphisms — CYP2C9 (C430T and A1075C), VKORC1. The method provided for the simultaneous detection of two allelic variants of each polymorphism in one reaction. DNA extraction was performed according to the instructions for the reagent kit, using the PROBA-RAPID-GENETICS kit for isolating nucleic acids from biological samples (NPO DNA-Technology, Russia). For each polymorphism, the required number of tubes were prepared, which were then shaken with the amplification mixture and centrifuged for 3 seconds in a Vortex microcentrifuge. To each tube were added 20 μl of the amplification mixture prepared from a mixture of PCR buffer and TechnoTaq MAX-AT polymerase in a ratio of 10 μl and 0.5 μl, respectively. After mixing, the mixture was centrifuged. To each tube were added 10 μl of the prepared DNA sample and 20 μl of mineral oil to exclude cross-contamination, after which it was centrifuged again. Then 5 μl of the DNA sample were added to each reaction tube, after which repeated centrifugation was performed. As a control, 5 μl of the negative sample was used. All tubes were placed in the Dtlite amplifier block, where the RealTime PCR program was launched, automating the reaction. The program included initial denaturation at 95 °C for 3 min, followed by 40 cycles: denaturation at 95 °C for 15 seconds and annealing at 63 °C for 40 seconds. After the reaction was completed, the results were recorded. Based on the results of the study, a conclusion was made for each participant with the determination of genotypes for CYP2C9 (C430T and A1075C), VKORC1 polymorphisms. Statistical analysis was performed using the StatTech v. 4.8.5 program (Stattech LLC, Russia). Quantitative indicators were assessed for compliance with the normal distribution using the Kolmogorov-Smirnov criterion. The description of quantitative characteristics in case of normal distribution is presented as the arithmetic mean ± standard deviation (M±SD, the boundaries of the 95% confidence interval (95% CI) were indicated as a measure of representativeness for mean values), and as the median with the 25th and 75th percentiles (Me [Q1; Q3]) — for a distribution different from normal. Comparison of two groups by a quantitative indicator, the distribution of which differed from normal, was performed using the Mann–Whitney U test, and comparison of three or more groups — using the Kruskal–Wallis test. Comparison of percentages in the analysis of four-field contingency tables was performed using Fisher's exact test. As a quantitative measure of effect when comparing relative indicators, the odds ratio with a 95% confidence interval (OR; 95% CI) was calculated. Comparisons of percentages in the analysis of multifield contingency tables were performed using the Pearson chi-square test. Post hoc comparisons were performed using the Pearson chi-square test with Holm's correction.
Results
The study included 74 patients of Chuvash nationality with CRHD, observed at the BUK Cheboksary Regional Clinical Hospital from May 2023 to February 2024. The average age of the study participants was 66.4 years (Q1–Q3: 62.00–70.75 years). Most patients were female, their proportion reached 62.2% (n=46). All patients examined had hypertension and chronic heart failure as concomitant pathology, more than 70% had atrial fibrillation and hyperlipidemia. More than 75% of patients had mechanical prostheses of one or more heart valves [25]. Mitral valve stenosis was frequently detected - in 77% of those examined, aortic valve stenosis was diagnosed in 59.5%, and tricuspid valve stenosis in 18.9%. Almost all study participants had calcification or thickening of the heart valves (Table 1), and lesions of several valves were often recorded.
Table 1
The incidence of calcification of the valve apparatus of the heart in the studied patients–Chuvash with chronic rheumatic heart disease (n=74)
Кальциноз клапанов сердца | n | % | 95 % ДИ |
Аортальный / Митральный /Трёхстворчатый | 56 | 75,7 | 64,3–84,9 |
Аортальный | 37 | 50,0 | 38,1–61,9 |
Митральный | 34 | 45,9 | 34,3–57,9 |
Трёхстворчатый | 3 | 4,1 | 0,8–11,4 |
The obtained results of pharmacogenetic testing (Table 2) corresponded to those expected according to the Hardy–Weinberg equation, p>0.05 (CYP2C9*2: χ2=0.941, p=0.332; CYP2C9*3: χ2=0.132, p=0.716; VKORC1: χ2=0.51, p=0.821; CYP4F2: χ2=0.560, p=0.454), which indicates that the distribution of genotype frequencies in this sample of patients reflects their distribution in the population.
Table 2
Carriage of gene polymorphisms in Chuvash patients with chronic rheumatic heart disease (n=74)
Ген и его варианты | Количество пациентов-чувашей (n) и доля (%) носителей варианта гена | ||
n | % | 95 % ДИ | |
CYP2C9*2:_430_C>T |
|
| |
СС | 59 | 79,7 | 68,8–88,2 |
СТ | 15 | 20,3 | 11,8–31,2 |
ТТ | не выявлено | ||
Минорный аллель Т | 10,15 % | ||
CYP2C9*3:_A>C | |||
AA | 68 | 91,9 | 83,2–97,0 |
AC | 6 | 8,1 | 3,0–16,8 |
СС | не выявлено | ||
Минорный аллель С | 4,05 % | ||
VKORC1:_–1639_G>A | |||
GG | 20 | 27,0 | 17,4–38,6 |
GA | 36 | 48,6 | 36,9–60,6 |
AA | 18 | 24,3 | 15,1–35,7 |
Минорный аллель А | 48,6 % | ||
In the context of the conducted pharmaco-genotyping for the VKORC1 gene (–1639_G>A, rs9923231), the heterozygous GA variant was dominant, occurring in 48.6% of the subjects (n=36), while the homozygous AA allele was found in 24.3% (n=18), and the “wild” gene in 27% (n=20). Thus, the frequency of the A allele for this gene was 48.6% among Chuvash patients with CRHD. When studying the carriage of CYP2C9*2 variants (430 C>T, rs1799853), it was found that 79.7% (n=59) of patients did not have polymorphic variants, and 20.3% (n=15) had heterozygous forms of CT. Similarly, when analyzing the CYP2C9*3 variant (A>C, rs1057910), more than 91.9% (n=68) of patients had the "wild" gene, while the heterozygous AS variant was found in 8.1% (n=6). It should be noted that homozygous polymorphisms for these two genes were not detected.
Further analysis included the study of possible associations between the presence of polymorphic alleles of the studied genes and concomitant diseases such as coronary heart disease, hypertension, chronic heart failure, atrial fibrillation, and extrasystole. No statistically significant relationships were found. Attention was drawn to the association between the carriage of the VKORC1 gene polymorphism and the presence of calcification of the heart valves in Chuvash patients with CRHD. Thus, calcification of the valve apparatus was significantly more common (p=0.014, pAA–GA=0.030) in homozygous carriers of the A allele than in heterozygous carriers or in the absence of the A allele (Fig. 1).
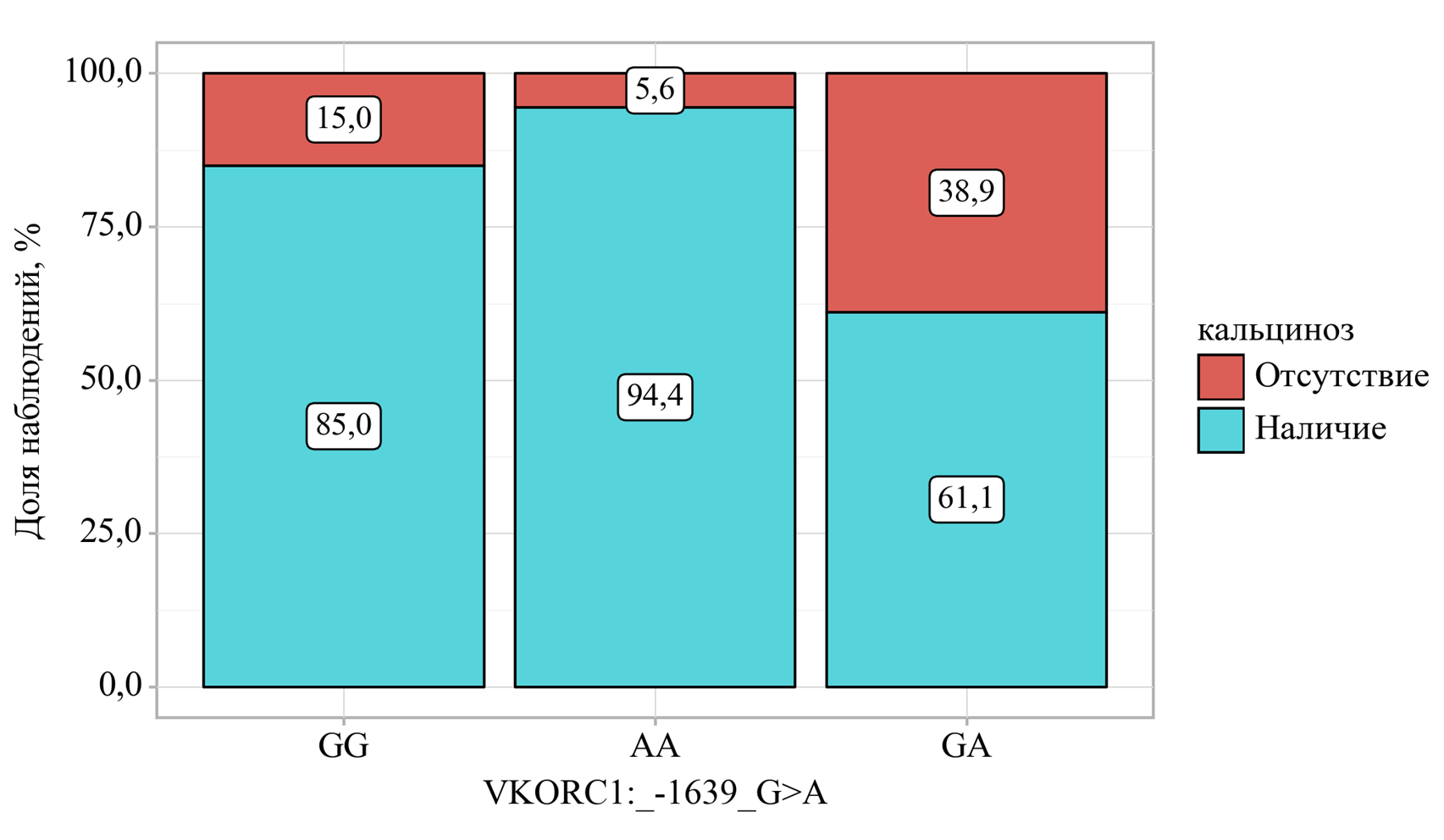
Fig. 1. Association between homozygous carriage of the AA allele of VKORC1 (−1639G>A) and calcification of heart valves in Chuvash patients with CRHD (n=74)
A more detailed study further demonstrated the presence of a connection between homozygous carriage of the AA allele of VKORC1 (−1639G>A) with calcification of the aortic valve (p=0.023, pAA–GA=0.021), but not the mitral valve (p=0.030, pGG–GA=0.025), while no significant associations with calcification of the tricuspid valve were found (p=0.860) (Fig. 2).
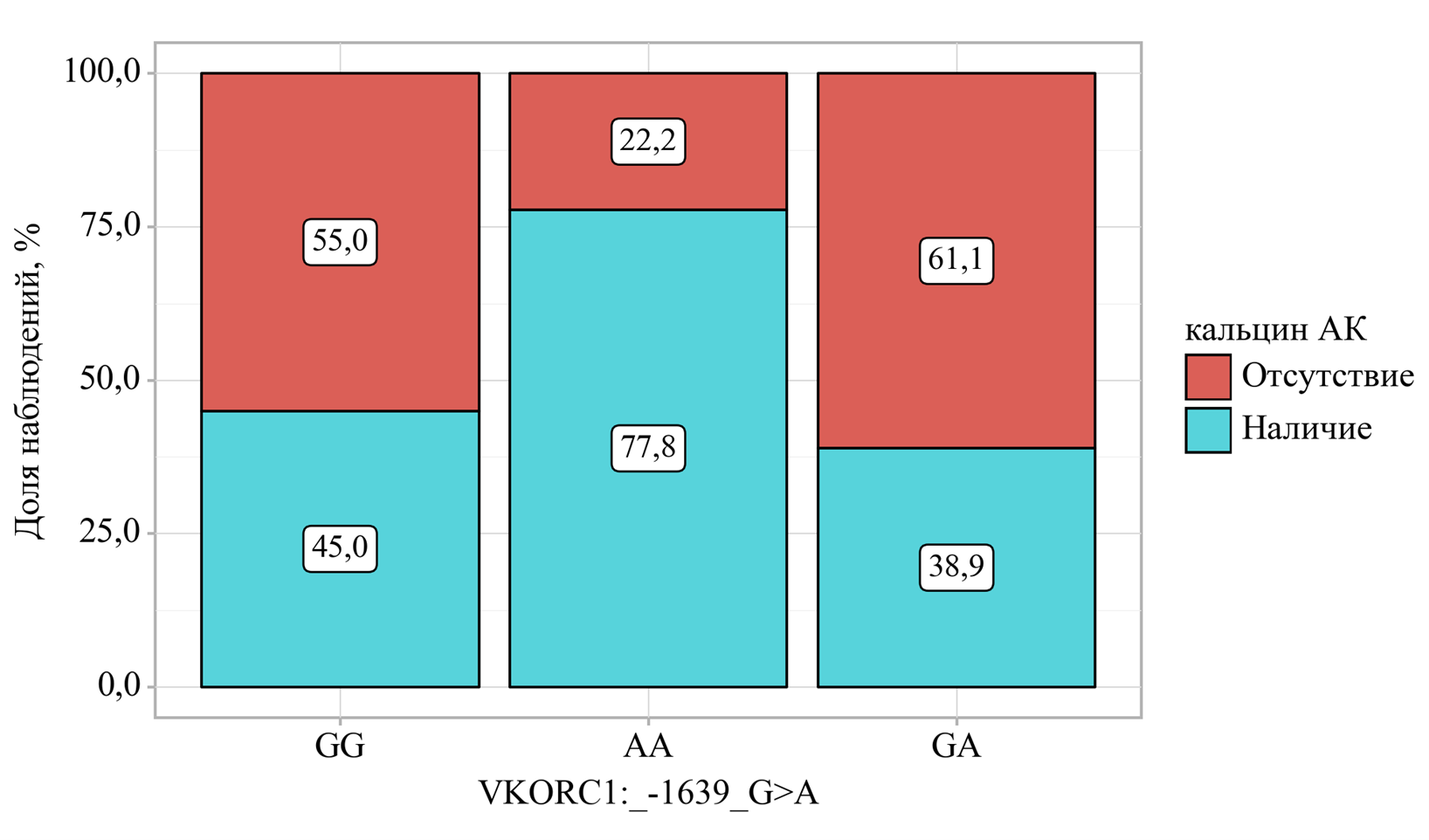
Fig. 2. Association between the carriage of VKORC1 gene polymorphisms (−1639G>A) and calcification of the aortic valves of the heart (p=0.023, pAA–GA=0.021) in chuvash patients with CRHD (n=74).
Discussion
A prospective study was conducted, which included 74 patients of the Chuvash ethnic group diagnosed with CRHD; women predominated in terms of gender composition. Despite the fact that 24.3% of patients did not have prosthetic valves, all patients had indications for anticoagulant therapy and received warfarin due to the risk of thrombosis.
It is well known that sensitivity to warfarin is largely associated with polymorphisms of the VKORC1 and CYP2C9 genes, the carriage of which has ethnic and geographic differences [5–23]. Literature data indicate that the minor allele A of the polymorphic variant of the VKORC1 gene (−1639G>A) is very often (more than 90% of the population) detected in Japan and China (Han Dynasty) [4–7], and, conversely, is relatively rare among the population of black Americans and Indians [21]. In the present study, polymorphisms of the VKORC1 gene (−1639G>A) were not uncommon among Chuvash patients with CRHD. The results of the analysis demonstrated that the heterozygous GA status was found in half of the participants (48.6%), the homozygous AA form in 18%, and the “wild” variant in 27%. In general, the frequency of the minor allele A of the VKORC1 gene in the Chuvash population was 48.6%, which is comparable with data for the population of Argentina, Syria, Egypt, Turkey and Italy [9, 10, 13, 16, 19], where the frequency of the A allele was from 47 to 56%. Among the genetic factors that increase sensitivity to warfarin, the carriage of genetic variants of CYP2C9 is also of great clinical significance. As part of the genotyping for CYP2C9*2 and CYP2C9*3 carriage in Chuvash patients with CRHD, the dominance of "wild" gene variants was demonstrated - 79.7 and 91.9% over polymorphic ones, while homozygous polymorphisms were not detected. It should be noted that all Chuvash patients with CRHD included in the study received the anticoagulant warfarin. The pharmacodynamics of this anticoagulant is aimed at inhibiting the VKORC1 enzyme. Thus, warfarin prevents post-translational modification of various proteins dependent on vitamin K: it can disrupt the activation of not only coagulation factors in the liver, but also matrix Gla protein (MGP), which is a potent inhibitor of vascular calcification [23]. On the one hand, carriage of VKORC1 polymorphisms increases the anticoagulant effect of warfarin, but on the other hand, it is possible to assume that this may be a factor in the development of calcification of both elastic vessels and the associated heart valves, which are affected in CRHD. Data obtained in a number of experimental and clinical studies indicate that a decrease in the activity of the VKORC1 enzyme can affect the processes of calcification of the vascular walls. For example, a study on rats showed that the use of warfarin causes a significant increase in the concentration of calcium in the tissues of elastic vessels, including the aorta [26]. At the same time, a diet rich in vitamin K1 slowed the progression of calcification. Genetically determined decrease in VKORC1 activity was also associated with vascular calcification. Thus, an association was found between the presence of the polymorphic T-allele of VKORC1 (1173 C>T) and an increased risk of aortic calcification in representatives of the Caucasian race [13]. Carriers of this allele demonstrated a 19% higher risk of developing calcification compared to carriers of the "wild" type. Pathogenetically, this may be associated with inhibition of the formation of active MGP, which promotes the accumulation of calcium in the walls of blood vessels and valves, which is clinically manifested in the development of calcification [25-28]. Almost all Chuvash patients with CRHD examined by us had signs of calcification and / or thickening of the heart valves according to the results of echocardiography and ultrasound. In this regard, an analysis of the relationship between the carriage of polymorphic variants of the studied genes with the presence of calcification of the heart valves was carried out. A statistically significant association of valve calcification was found with the studied VKORC1 polymorphism, but not CYP2C9. In the course of the study, we found a significant association between the carriage of homozygous polymorphism of the VKORC1 gene (G1639A) and calcification of the heart valves, as well as calcification of the aortic valve, but not other valves separately. Thus, our data may indicate that a genetically determined decrease in VKORC1 activity may be associated with an increased risk of valve calcification (mainly aortic) in patients taking warfarin. These results further emphasize the importance of taking into account genetic and pharmacological factors in the clinical assessment of vascular calcifications and may be important for the development of individualized strategies for anticoagulant therapy of patients with CRHD.
Study limitation
The power of this study should be considered insufficient. However, despite the fact that only 74 patients participated in the study, the results of pharmacogenetic testing were consistent with those expected according to the Hardy-Weinberg equation, which indicates the possible extrapolation of the findings to the population.
Conclusion
1. Among patients of the Chuvash population with CRHD, the frequency of the A allele of the VKORC1 polymorphic gene (−1639G>A) was 48.60%, the T allele of CYP2C9*2 was 10.15%, and the C allele of CYP2C9*3 was 4.05%. Homozygous polymorphisms of CYP2C9*2 and CYP2C9*3 were not detected among Chuvash patients with CRHD.
2. 75.7% of patients with CRHD were diagnosed with calcification of any heart valve, most often calcification of the aortic (50%) and mitral (45.9%) valves, less often - tricuspid (4.1%). 3. Among homozygous carriers of the A allele of the VKORC1 gene (-1639G>A) in patients of the Chuvash ethnic group with CRHD, calcification of the heart valves is more often observed. A reliable association was revealed between homozygous carriage of the minor A allele of the VKORC1 gene (-1639G>A) and calcification of the aortic heart valve (p = 0.023, pAA–GA = 0.021).
References
1. Prikladnaya farmakogenetika : Monografiya / Ed by DA Sycheva Moscow. Tver': OOO Izdatel'stvo “Triada”, 2021. (In Russ.)
2. Teh LK, Langmia IM, Fazleen Haslinda MH, et al. Clinical relevance of VKORC1 (G-1639A and C1173T) and CYP2C9*3 among patients on warfarin. J Clin Pharm Ther. 2012 Apr;37(2):232-6. doi: 10.1111/j.1365-2710.2011.01262.x.
3. Schurgers LJ, Teunissen KJ, Knapen MH, et al. Novel conformation-specific antibodies against matrix gamma-carboxyglutamic acid (Gla) protein: undercarboxylated matrix Gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol. 2005 Aug;25(8):1629-33. doi: 10.1161/01.ATV.0000173313.46222.43.
4. Qayyum A, Najmi MH, Mansoor Q, et al. Frequency of Common VKORC1 Polymorphisms and Their Impact on Warfarin Dose Requirement in Pakistani Population. Clin Appl Thromb Hemost. 2018 Mar;24(2):323-329. doi: 10.1177/1076029616680478.
5. Yoshizawa M, Hayashi H, Tashiro Y, et al. Effect of VKORC1-1639 G>A polymorphism, body weight, age, and serum albumin alterations on warfarin response in Japanese patients. Thromb Res. 2009 Jun;124(2):161-6. doi: 10.1016/j.thromres.2008.11.011.
6. Obayashi K, Nakamura K, Kawana J, et al. VKORC1 gene variations are the major contributors of variation in warfarin dose in Japanese patients. Clin Pharmacol Ther. 2006 Aug;80(2):169-78. doi: 10.1016/j.clpt.2006.04.010.
7. Miao L, Yang J, Huang C, Shen Z. Contribution of age, body weight, and CYP2C9 and VKORC1 genotype to the anticoagulant response to warfarin: proposal for a new dosing regimen in Chinese patients. Eur J Clin Pharmacol. 2007 Dec;63(12):1135-41. doi: 10.1007/s00228-007-0381-6.
8. Mazzaccara C, Conti V, Liguori R, et al. Warfarin anticoagulant therapy: a Southern Italy pharmacogenetics-based dosing model. PLoS One. 2013 Aug 26;8(8):e71505. doi: 10.1371/journal.pone.0071505.
9. Cini M, Legnani C, Cosmi B, et al. A new warfarin dosing algorithm including VKORC1 3730 G > A polymorphism: comparison with results obtained by other published algorithms. Eur J Clin Pharmacol. 2012 Aug;68(8):1167-74. doi: 10.1007/s00228-012-1226-5.
10. Scibona P, Redal MA, Garfi LG, et al. Prevalence of CYP2C9 and VKORC1 alleles in the Argentine population and implications for prescribing dosages of anticoagulants. Genet Mol Res. 2012 Jan 9;11(1):70-6. doi: 10.4238/2012.January.9.8.
11. Wang TL, Li HL, Tjong WY, et al. Genetic factors contribute to patient-specific warfarin dose for Han Chinese. Clin Chim Acta. 2008 Oct;396(1-2): 76-9. doi: 10.1016/j.cca.2008.07.005.
12. Liang R, Li L, Li C, et al. Impact of CYP2C9*3, VKORC1-1639, CYP4F2rs2108622 genetic polymorphism and clinical factors on warfarin maintenance dose in Han-Chinese patients. J Thromb Thrombolysis. 2012 Jul;34(1):120-5. doi: 10.1007/s11239-012-0725-7.
13. Botton MR, Bandinelli E, Rohde LE, et al. Influence of genetic, biological and pharmacological factors on warfarin dose in a Southern Brazilian population of European ancestry. Br J Clin Pharmacol. 2011 Sep;72(3):442-50. doi: 10.1111/j.1365-2125.2011.03942.x.
14. Altawil Y, Youssef LA. Frequencies of VKORC1-1639G>A and rs397509427 in Patients on Warfarin and Healthy Syrian Subjects. Cardiovasc Ther. 2023 Nov 23;2023:8898922. doi: 10.1155/2023/8898922.
15. Kumar DK, Shewade DG, Surendiran A, Adithan C. Genetic variation and haplotype structure of the gene Vitamin K epoxide reductase complex, subunit 1 in the Tamilian population. J Pharmacol Pharmacother. 2013 Jan;4(1):53-8. doi: 10.4103/0976-500X.107683.
16. Nahar R, Deb R, Saxena R, et al. Variability in CYP2C9 allele frequency: a pilot study of its predicted impact on warfarin response among healthy South and North Indians. Pharmacol Rep. 2013;65(1):187-94. doi: 10.1016/s1734-1140(13)70977-0.
17. Bazan NS, Sabry NA, Rizk A, et al. Factors affecting warfarin dose requirements and quality of anticoagulation in adult Egyptian patients: role of gene polymorphism. Ir J Med Sci. 2014 Jun;183(2):161-72. doi: 10.1007/s11845-013-0978-y.
18. Namazi S, Azarpira N, Hendijani F, et al. The impact of genetic polymorphisms and patient characteristics on warfarin dose requirements: a cross-sectional study in Iran. Clin Ther. 2010 Jun;32(6):1050-60. doi: 10.1016/j.clinthera.2010.06.010.
19. Özer M, Demirci Y, Hizel C, et al. Impact of genetic factors (CYP2C9, VKORC1 and CYP4F2) on warfarin dose requirement in the Turkish population. Basic Clin Pharmacol Toxicol. 2013 Mar;112(3):209-14. doi: 10.1111/bcpt.12024.
20. Gan GG, Phipps ME, Lee MM, et al. Contribution of VKORC1 and CYP2C9 polymorphisms in the interethnic variability of warfarin dose in Malaysian populations. Ann Hematol. 2011 Jun;90(6):635-41. doi: 10.1007/s00277-010-1119-6.
21. Rusdiana T, Araki T, Nakamura T, et al. Responsiveness to low-dose warfarin associated with genetic variants of VKORC1, CYP2C9, CYP2C19, and CYP4F2 in an Indonesian population. Eur J Clin Pharmacol. 2013 Mar;69(3):3 95-405. doi: 10.1007/s00228-012-1356-9.
22. Wang D, Chen H, Momary KM, et al. Regulatory polymorphism in vitamin K epoxide reductase complex subunit 1 (VKORC1) affects gene expression and warfarin dose requirement. Blood. 2008 Aug 15;112(4):1013-21. doi: 10.1182/blood-2008-03-144899.
23. Teichert M, Visser LE, van Schaik RH, et al. Vitamin K epoxide reductase complex subunit 1 (VKORC1) polymorphism and aortic calcification: the Rotterdam Study. Arterioscler Thromb Vasc Biol. 2008 Apr;28(4):771-6. doi: 10.1161/ATVBAHA.107.159913.
24. Results of the All-Russian Population Census 2020. Volume 5. (In Russ.) https://rosstat.gov.ru/storage/mediabank/Tom5_tab1_VPN–2020.xlsx
25. Georgieva KS, Pavlova SI, Maksimov ML. Carriage of CYP2C9, VKORC1 and CYP4F2 gene polymorphisms in chuvash patients with chronic rheumatic heart disease. Krymskii zhurnal eksperimental'noi i klinicheskoi meditsiny. 2024;14(4):20-29. (In Russ.) doi: 10.29039/2224-6444-2024-14-4-20-29.
26. McCabe KM, Booth SL, Fu X, et al. Dietary vitamin K and therapeutic warfarin alter the susceptibility to vascular calcification in experimental chronic kidney disease. Kidney Int. 2013 May;83(5):835-44. doi: 10.1038/ki.2012.477.
27. Price PA, Faus SA, Williamson MK. Warfarin causes rapid calcification of the elastic lamellae in rat arteries and heart valves. Arterioscler Thromb Vasc Biol. 1998 Sep;18(9):1400-7. doi: 10.1161/01.atv.18.9.1400.
28. Lacombe J, Ferron M. Gamma-carboxylation regulates osteocalcin function. Oncotarget. 2015 Aug 21;6(24):19924-5. doi: 10.18632/oncotarget.5126.
About the Authors
K. S. GeorgievaRussian Federation
Ksenia S. Georgieva, Assistant Professor
Department of Pharmacology, Clinical Pharmacology, and Biochemistry
Cheboksary
Competing Interests:
The authors declare no conflict of interest
S. I. Pavlova
Russian Federation
Svetlana I. Pavlova, Head of the Department
Department of Pharmacology, Clinical Pharmacology, and Biochemistry
Cheboksary
Competing Interests:
The authors declare no conflict of interest
What is already known on this topic?
- Sensitivity to warfarin is individual and highly dependent on genetic polymorphisms, primarily of the CYP2C9 gene (responsible for drug metabolism) and the VKORC1 gene (its target).
- By blocking VKORC1, warfarin inhibits not only the synthesis of clotting factors but also the activation of matrix Gla protein (MGP)—a powerful inhibitor of vascular calcification.
- This links warfarin therapy to the risk of vascular calcification.
- Chronic rheumatic heart disease (CRHD) itself is characterized by progressive calcification of the heart valves.
- The frequency of VKORC1 and CYP2C9 alleles has significant ethnic variations, but data on the Chuvash population were limited.
What does the study add?
- This is the first report of allele frequencies of key pharmacogenetic markers (VKORC1 −1639G>A, CYP2C9*2, CYP2C9*3) specifically in Chuvash patients with CRHD.
- VKORC1 A allele: 48.6%
- T allele (CYP2C9*2): 10.15%
- C allele (CYP2C9*3): 4.05%
- A novel association was established: in this patient cohort, homozygous carriage of the A allele (AA genotype) of the VKORC1 gene was significantly associated with the development of aortic valve calcification (p=0.023).
- The very high prevalence of valve calcification (75.7%) in patients with CRHD was confirmed, with the aortic (50%) and mitral (45.9%) valves most commonly affected.
How might this affect clinical practice in the foreseeable future?
- The obtained data support the feasibility of pharmacogenetic testing in Chuvash patients with CRHD before prescribing warfarin.
- The test results could help personalize anticoagulant therapy. For carriers of the VKORC1 AA genotype, when choosing therapy, a physician would consider not only the increased risk of bleeding due to hypersensitivity to warfarin but also a potentially higher risk of progression of aortic valve calcification.
- This may tip the scales in favor of considering warfarin-alternative anticoagulants (DOACs), if there are no other contraindications (e.g., the presence of a mechanical valve prosthesis), especially in patients with already established calcification.
- For patients who continue warfarin therapy, knowing the genotype will allow for more precise dose titration and enhanced monitoring of the valvular apparatus using echocardiography.
Review
For citations:
Georgieva K.S., Pavlova S.I. Polymorphisms of CYP2C9 and VKORC1 genes and their association with calcification of heart valves in Chuvash patients with chronic rheumatic heart disease. Pharmacogenetics and Pharmacogenomics. 2025;(1):17-23. (In Russ.) https://doi.org/10.37489/2588-0527-2025-1-17-23. EDN: BXYGEA











































